Types of Diabetes
Type 1 (autoimmune disease/usually diagnosed to children): The pancreas makes no insulin or so little insulin that the body can’t use blood sugar for energy. Type 1 diabetes must be controlled with daily insulin.
Type 2 (usually diagnosed to adults): The body either makes too little insulin or can’t use the insulin it makes to use blood sugar for energy. Sometimes Type 2 diabetes can be controlled through eating a proper diet and exercising regularly. Many people with type 2 diabetes have to take diabetes pills, insulin, or both.
Gestational: Diagnosed in a pregnant woman who did not have diabetes before she was pregnant. Around 20-weeks, the placenta creates insulin resistance in the mother cells. If there isn’t an increase in insulin production, then you have too much glucose/sugar floating around. Often gestational diabetes can be controlled through eating a healthy diet and exercising regularly. Sometimes a woman with gestational diabetes must also take insulin.
Planning pregnancy and preventing gestational diabetes
It is always best to plan for pregnancy, but especially when you’re navigating life with an illness. If you know you have diabetes, do your best to plan your pregnancy to closely manage your diabetes. You may want to consult a doctor and a nutritionist as part of your preparation. Note, you may be advised on getting rid of weight to be in more control of your blood sugar.
When planning to have a baby, regardless if you have diabetes or not, it’s important to manage and maintain an appropriate weight for your body (before conception, throughout pregnancy, and postpartum). This means exercise and managing your eating habits are vital. Practice eating less sugar, no added sugars, implementing sugar replacements (like agave and natural honey), carb replacements, and meet with a nutritionist who can help you make accommodations so that you can enjoy the foods that you like, alongside eating a healthy meals. We can enjoy our foods, while taking care of our body and baby.
It is important to be familiar with your body, how it reacts to certain foods and how it responds to your exercising practices.
Testing for gestational diabetes
Every woman in pregnancy is offered a gestational test. The test is referred to as a glucose tolerance test (GTT). If you test positive, your pregnancy will be labeled as high risk.
What is referred to as gestational diabetes may actually be Type 2 diabetes because it’s not often that people are taking diabetes test. The glycated hemoglobin test (A1C/HbA1C) is a reading of what’s occurring during the first trimester (2-3 months), which is not picking up gestational diabetes because the pregnancy changes—in this instance— have yet to happen. If you take the oral GTT and receive positive results of gestational diabetes, it’s more likely to be Type 2 diabetes (most likely previously undiagnosed).
Your provider most likely won’t mention this to you, but you can test your own glucose levels. Yes, self-testing is an option! You may purchase a test at Walgreens, CVS, Walmart, Target, etc. Over a few days, you would check your own glucose levels. Try taking your blood pressure when you first wake up, an hour after eating, two hours after eating, and before going to sleep consistently during this timespan of testing.
If you are diagnosed with gestational diabetes, this could be a sign/warning of future increased health concerns (such as cardiovascular disease, Type 2 diabetes, and potentially more). The positive results are providing a general sense of your health and your body’s ability to produce insulin (during pregnancy and beyond). The higher the glucose levels, the higher a chance for having a big baby.
Understanding glucose level numbers
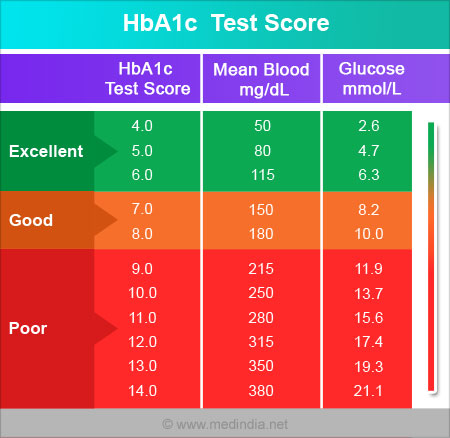
Target for women testing blood glucose levels during pregnancy:
- Before a meal: 95 mg/dl or less
- One hour after a meal: 140 mg/dl or less
- Two hours after a meal: 120 mg/dl or less
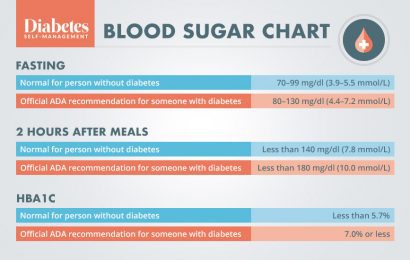
Why have we reduced the limits compared to when you’re not pregnant? Because you have 1.75 times the chance of having a big baby, if your blood glucose levels are above 5.1. What is considered a big baby and how can we tell what is a big baby? It’s about making baby’s smaller (4oz. or more).
Things to consider and be mindful of during pregnancy
- Placenta hormones can cause high blood sugar. When getting an ultrasound, ask questions about the health of the placenta.
- Preeclampsia (high blood pressure)
- Hypoglycemia (low blood pressure)
- Premature birth
- Your baby gaining excessive weight / your baby being too big. Babies tend to store the fat at the top end (the chest and abdomen of the baby grows more rounded). When there is gestational diabetes, the growth of the baby may not actually be where they need to be. This can cause shoulder dystocia (for the baby), which can result in fetal injury or fetal death. For the mother this can cause perineal tearing (potentially an excessive tear). Kiara Fair, RN, MSN says, “Shoulder dystocia contrary to popular belief is often caused by epidurals and poor fetal positioning in the maternal pelvis. Many doctors and midwives alike scare patients with big babies with shoulder dystocia and blame it on the size of the baby when in fact research from outside the US and some US shows it’s from epidural and poor positions not from large babies. Delivering and pushing on the back is a major culprit of shoulder dystocia due to poor fetal rotation in the maternal pelvis. Decrease chances of shoulder dystocia through increasing the diameter of the maternal pelvis through upright positions like squatting and lunging.”
- C- Section (Cesarean Section)
- Birth defects
- Miscarriage or stillbirth
At 20-weeks, the fetus is fully formed and is more-so focused on getting bigger and stronger. So any high blood glucose levels interfere with/change the growth of the baby. If you have high blood glucose levels from pre-conception or early gestation, then it increases morbidity, miscarriage, or stillbirth.
Being induced
Your provider may schedule you for a routine induction because you are labeled high risk with diabetes; even if there’s no increased chance that anything is negatively happening or impacting you or your baby. We’ve got guidelines, including The World Health Organization stating that: If a woman has been diagnosed with gestational diabetes and has maintained normal blood glucose levels, she should not be induced for gestational diabetes because she’s not going to have a bigger baby (if you think that’s a problem), which is not necessarily a problem. But if you think the big baby is a problem—if her blood glucose levels are normal, then she’s not going to have a bigger baby because of her glucose levels. So why are you inducing her?
Dr Rachel Reed, The Midwives’ Cauldron Podcast episode: Gestational diabetes: the pregnancy perspective
Induction Chances
- Besides the baby being too big, what causes shoulder dystocia? An induction causes a baby to ram in the pelvis before the baby naturally does what’s needed to move through the pelvis, transition, and navigate their way into this realm.
- increases chance of minimum movement
- epidural
- c-section
- postpartum hemorrhaging
They say big babies are dangerous. Are big babies dangerous or is it provider interventions that causes complications?
How are we defining big babies? in terms of is it accurate? how will we definite it? what is considered big and how accurate are the scans?
The scans are not accurate. You can’t tell the size of a baby from a scan. There’s good evidence to support that statement. We keep doing it, but we can’t actually tell. So we can’t tell that there’s a big baby based on a scan. So big babies are 4kilos (8.8lbs) or over and so is considered big baby.
Part of the problem is that when research is done … then they include women who have had babies because of blood glucose levels and women who just have big babies because that’s what they grow (genetically).
If the baby is estimated to be 8lbs on ultrasound, it can be anywhere between 6.30 and 9.3.
So you cannot estimate the size of a baby and if you’re worried about the size of the baby (in terms of it being too small), then that is then about growth restriction. Because you’re not worried about a genetically small baby. What you’re worried about is if the placenta is not actually feeding the baby. So scanning for the size of the baby doesn’t help with that. You need to actually scan and look at what the placenta is doing. So let’s stop scanning babies to guess at their size.
Dr Rachel Reed, The Midwives’ Cauldron Podcast episode: Gestational diabetes: the pregnancy perspective
It’s safe and normal for babies to weigh more than 8lbs by the time of delivery.
[Regardless of the size, babies will] slip right out with the right positions. I have witnessed so many tiny ladies (4’10-5’2 ft tall) deliver really big babies like it’s nothing.
The only big babies I’ve had issues with are diabetic. Only had one shoulder dystocia of a client who was not diabetic and did not have a big baby, but I think that one was due to epidural.
Kiara Fair, RN, MSN Healing Hands Birth & Women’s Services
There is much more to cover, but remember
You may be labeled as high risk if you’re pregnant with diabetes, but it does not mean that you can’t have the birth that you desire. You have birth rights and always have the right to choose.
Source
- 1 American Diabetes Association: Gestational diabetes and a healthy baby?
- 2Kiara Fair, RN, MSN Healing Hands Birth & Women’s Services
- Problems of Diabetes in Pregnancy
- Majority of this article is written from The Midwives’ Cauldron podcast, episode: Gestational diabetes: the pregnancy perspective